Technologies
Total Hemoglobin (SpHb®)
A noninvasive way to help clinicians monitor hemoglobin trends continuously and in real time.
Limits of Traditional Methods Alone
Invasive blood samples provide intermittent and delayed hemoglobin results.
How Does SpHb Work?
Part of the rainbow® technology suite of noninvasive measurements, SpHb leverages multiple wavelengths of light via a Pulse CO-Oximetry sensor to acquire blood constituent data through light absorption.
Advanced signal processing algorithms and unique adaptive filters work together to offer hemoglobin (SpHb) and oxygen saturation (SpO2), in addition to methemoglobin (SpMet®), pulse rate (PR), perfusion index (Pi), pleth variability index (PVi®), and other parameters – all in real time.
With greater visibility of blood constituents, rainbow® SpHb enables clinicians to monitor changes in hemoglobin between invasive blood samples.
SpHb trend monitoring may provide additional insight between invasive blood samples when:
- The SpHb trend is stable and the clinician may otherwise think hemoglobin is dropping.
- The SpHb trend is rising and the clinician may otherwise think hemoglobin is not rising fast enough.
- The SpHb trend is dropping and the clinician may otherwise think hemoglobin is stable.
“Having continuous access to Hgb [hemoglobin] levels in real time offers a clear advantage over the traditional measurement methods as it enables clinicians to detect changes in Hgb levels quickly and adjust clinical management strategies accordingly."2
- Society for the Advancement of Patient Blood Management (SABM) Whitepaper, Improvement of Patient Outcomes with Hemoglobin Monitoring in the Critical Care and Perioperative Setting.
How Accurate is SpHb?
- With RD rainbow SET® sensors* the SpHb accuracy specification is ARMS** 1 g/dL in the range of 8-17 g/dL.
- Our latest sensor features improved trending across the SpHb measurement range.3
- For patients greater than 3 kg
- ARMS accuracy is a statistical calculation of the difference between device measurements and reference measurements. Approximately two-thirds of the device measurements fell within ± ARMS of the reference measurements in a controlled study.
-
Case Example
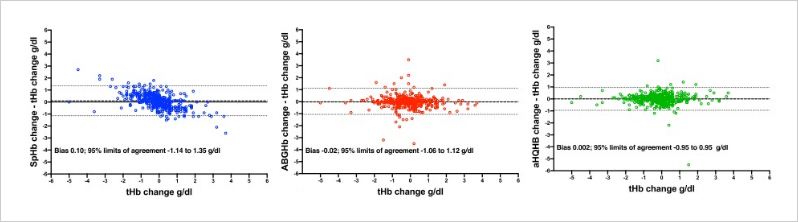
Multi-center Study Evaluating SpHb Accuracy
A multicenter study by Dr. Applegate and researchers from Loma Linda University in California, the University of California at Irvine, and the Mayo Clinic in Jacksonville, Florida, evaluated the trend accuracy of three hemoglobin (Hb) monitoring methods, including noninvasive, continuous SpHb.4
Fig. 1
Modified Bland–Altman analysis of trend accuracy comparing 416 sequential changes in laboratory hematology analyzer hemoglobin (tHb) to the difference between tHb changes and paired sequential changes. In the left panel: Pulse CO-Oximetry hemoglobin (SpHb); in the middle panel: arterial blood gas CO-Oximetry hemoglobin (ABGHb); in the right panel: Hemocue point-of-care hemoglobin using arterial blood (aHQHb). Horizontal dotted lines indicate 95% limits of agreement (± 1.96 SD).

Improve Care Team Efficiencies
SpHb can be displayed on Masimo and select third-party monitors, such as devices from Philips, GE, and Draeger, with the use of a multi-wavelength Masimo rainbow® Pulse CO-Oximetry sensor, which can help centralize patient data and increase its accessibility to care teams.
See our third-party monitor partners that offer rainbow® integrationImprove Patient Outcomes with SpHb
See evidence from around the world on how SpHb can support your blood management initiatives.
Clinical Applications
SpHb offers continuous, noninvasive monitoring of hemoglobin across a variety of cases.
Patient Blood Management
“Patient Blood Management is a patient-centered, systematic, evidence-based approach to improving patient outcomes by managing and preserving the patient’s own blood, while promoting patient safety and empowerment.”5
“The ultimate goal is not to treat a number, but to improve the outcomes of the patient, using a host of strategies described under Patient Blood Management to prevent and reduce the risk of anemia and manage it properly. Noninvasive Hgb monitoring devices can greatly contribute to this goal.”2
- SABM White Paper
“Measurement of Hb concentration is essential to estimate the severity of anemia; this information may be useful after a transfusion. This measurement can be done as part of a complete blood count, on blood gas specimens and by Pulse CO-Oximetry.”6
- Pediatric Critical Care Transfusion and Anemia Expertise Initiative (TAXI)
Blood and Fluid Monitoring
In addition to SpHb, the Masimo rainbow SET Pulse CO-Oximetry platform offers Pleth Variability Index, or PVi.
PVi is a measure of the dynamic changes in Perfusion Index (Pi) that occur during one or more respiratory cycles.
When monitored together, SpHb and PVi may provide clinicians with additional insight into a patient’s status.
Provided alongside SpHb on rainbow® Pulse CO-Oximetry sensors, PVi provides a continuous noninvasive measure of the relative variability in the photoplethysmograph (pleth) during respiratory cycles that may be used as a dynamic indicator of fluid responsiveness in select populations of mechanically ventilated adults.7
-
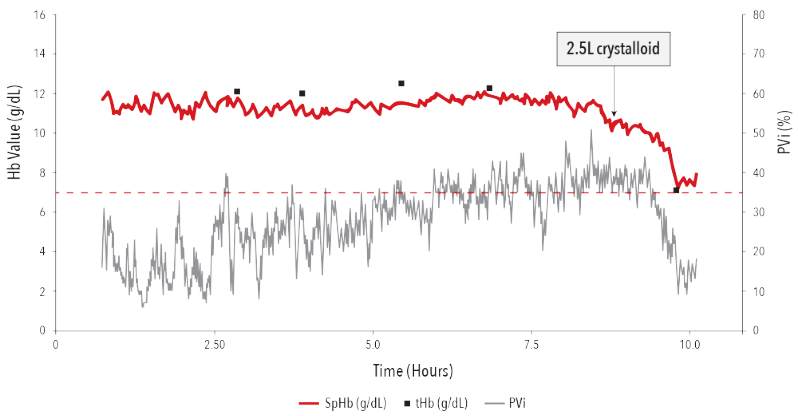
Case Example
SpHb Alongside PVi
The following hepatic surgery case depicts the effect of dilution on total hemoglobin upon the infusion of 2.5L of crystalloid.8
PVi and SpHb Support Clinicians in Improving Patient Outcomes
A single-center quality initiative involving 18,716 patients in the OR, ICU, and PACU was implemented in Limoges, France. The study used a Goal-directed Therapy (GDT) protocol with PVi in conjunction with a blood transfusion protocol based on SpHb.
Results demonstrated that monitoring with SpHb and PVi integrated in a vascular filling algorithm was associated with earlier transfusion and reduced 30- and 90-day mortality by 33% and 29%, respectively, on a whole hospital scale.9

Breakthrough Technology. Breakthrough Outcomes.
The study conducted at CHU Limoges, France demonstrated the clinical value of implementing a hospital-wide GDT protocol for blood and fluid management using Masimo noninvasive, continuous hemoglobin (SpHb), and pleth variability index (PVi) monitoring.9


Hemoglobin Spot-Checking
Quick, noninvasive SpHb spot-check monitoring is available with the handheld Rad-67® Pulse CO-Oximeter® and rainbow® DCI®-mini sensor.
Learn moreOutcome Studies
Multiple studies have demonstrated the value of continuous, noninvasive hemoglobin monitoring, SpHb.
-
Patient Outcomes
“Continuous hemoglobin and plethysmography variability index monitoring can modify blood transfusion practice and is associated with lower mortality.”9
Learn more -
Transfusion Management: Average Units of Blood Transfused
“Continuous and noninvasive hemoglobin monitoring reduces red blood cell transfusion during neurosurgery: a prospective cohort study.”10
Learn more“Postoperative patient blood management: transfusion appropriateness in cancer patients.”11
Learn more“Continuous hemoglobin measurement during frontal advancement operations can improve patient outcomes.”12
Learn more -
Transfusion Management: Appropriateness of Transfusion
“Monitoring of plethysmography variability index and total hemoglobin levels during cesarean sections with antepartum hemorrhage for early detection of bleeding.”13
Learn more“Postoperative noninvasive hemoglobin monitoring is useful to prevent unnoticed postoperative anemia and inappropriate blood transfusion in patients undergoing total hip or knee arthroplasty: a randomized controlled trial.”14
Learn more -
Transfusion Management: Time to Transfusion
“Continuous and noninvasive hemoglobin monitoring reduces red blood cell transfusion during neurosurgery: a prospective cohort study.”10
Learn more“The value of continuous noninvasive hemoglobin monitoring in intraoperative blood transfusion practice during abdominal cancer surgery.”15
Learn more -
Transfusion Management: Patients Transfused
“Continuous non-invasive hemoglobin monitoring during orthopedic surgery: a randomized trial.”16
Learn more“Targeted bleeding management guided by non-invasive haemoglobin measurement in surgical patients.”17
Learn more -
Cost Savings
“Economic analysis of the reduction of blood transfusions during surgical procedures while continuous hemoglobin monitoring is used.”18
Learn more
RD rainbow™ Sensors
Continuous, noninvasive hemoglobin is available on the RD rainbow sensor.

Resources & More
Want more information? Below are key resources for SpHb total hemoglobin monitoring.
Materials
Videos
Studies
Contact
Set Up Your Risk-Free Trial
Contact us today for more information on how to monitor with SpHb.
References
Macknet MR, et al. Presented at the 17th Annual Meeting for the Society for Technology in Anesthesia. 2007;STA-31.
Society for the Advancement of Patient Blood Management (SABM) Whitepaper, Improvement of Patient Outcomes with Hemoglobin Monitoring in the Critical Care and Perioperative Setting. 31 January 2021.
Barker SJ, et al. Anesth Analg. 2016 Feb;122(2):565-72.
Applegate RL, et al. J Clin Monit Comput. 2020 Oct;34(5):883-892
Shander A, et al. Anes Analg. 2022 Sep 1;135(3):476-488.
Doctor M., et al. Pediatr Crit Care Med. 2018; 19(9): S98-S113
Cannesson M, et al. J Cardiothorac Vas Anes. 2010. Jun;24(3):487-97.
Perel A. Crit Care. 2017;21:291.
Cros J, et al. J Clin Monit Comput. Aug 2019:1-9. Study utilized a goal-directed fluid therapy protocol with PVi® in conjunction with a blood transfusion protocol based on SpHb.
Awada WN et al. J Clin Monit Comput. (2015) 29:733–740
Merolle L, et al. Blood Transfus. 2020 Sep;18(5):359-365.
Saracoglu, A, et al. J Clin Monit Comput. 2022 Dec;36(6):1689-1695.
Elsakka A, et al. Egyptian Journal of Anaesthesia. Volume 33, Issue 1, 2017, Pages 5-8.
Nakamori E, et al. Geriatr Orthop Surg Rehabil. 2021 Nov 19;12:21514593211060575.
Kamal A, et al. Open J of Anesth. 2016 Mar; 6, 13-19.
Ehrenfeld JM, et al. J Blood Disorders Transf. 2014, 5:9.
Akdag S, et al. J Coll Physicians Surg Pak 2022; 32(10):1242-1248.
Ribed-Sánchez B, et al. Sensors (Basel). 2018 Apr 27;18(5).
Clinical decisions regarding red blood cell transfusions should be based on the clinician’s judgment considering among other factors: patient condition, continuous SpHb monitoring, and laboratory diagnostic tests using blood samples. SpHb monitoring is not intended to replace laboratory blood testing. Blood samples should be analyzed by laboratory instruments prior to clinical decision making.
The accuracy of PVi in predicting fluid responsiveness is variable and influenced by numerous patient, procedure, and device-related factors. PVi measures the variation in the plethysmography amplitude but does not provide measurements of stroke volume or cardiac output. Fluid management decisions should be based on a complete assessment of the patient’s condition and should not be based solely on PVi.
For professional use. See instructions for use for full prescribing information including indications, contraindications, warnings and precautions.
PLCO-006853/PLM-14678A-0723